From this week, patients in England will be able to get prescription-only treatment for seven common conditions at their local community pharmacy, without the need for a GP appointment or prescription.
The launch of the new Pharmacy First service will offer patients more choice in how and where they access care by making even better use of our highly trained community pharmacists.
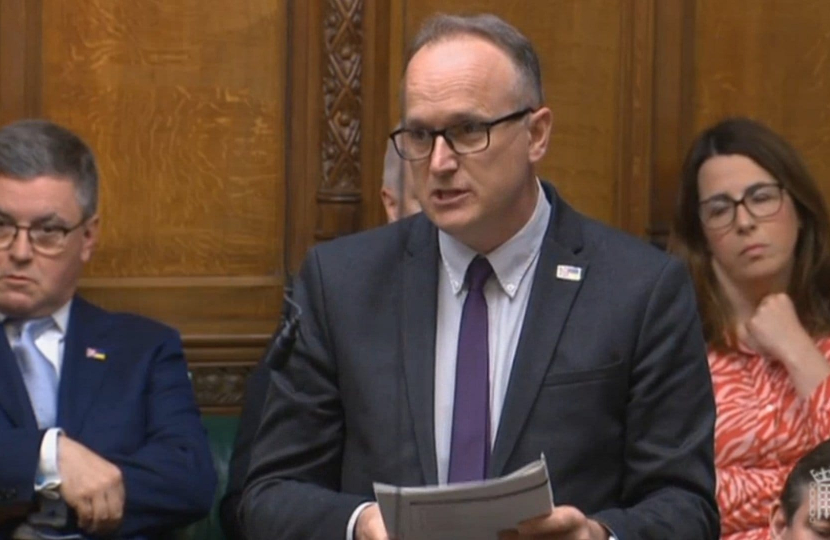
Dr Neil Hudson is dedicated to unlocking the potential of the 608 pharmacies already registered to deliver Pharmacy First services in the North East and North Cumbria Integrated Care Board's area.
Dr Neil Hudson MP said:
"Delivering for the health of my constituents and the health of the NHS, I am proud to support our Conservative Government's ambitious health agenda.
"Pharmacists are key individuals in healthcare - unlocking their potential is pivotal to delivering speedier treatment and opening up GP access."
Backed by up to £645 million, the expansion of community pharmacy is part of the Government's primary care recovery plan to make our NHS and social care system faster, simpler and fairer for us all.
For the first time ever, community pharmacies in England will be able to offer NHS consultations and supply prescription-only medicines without a prescription from a GP for seven common conditions. These conditions are sinusitis, sore throat, earache, infected insect bite, impetigo, shingles and uncomplicated urinary tract infections in women.
For these conditions, patients will be able to have a consultation with their pharmacist to discuss their symptoms. The pharmacist will then recommend the most clinically appropriate course of action abiding by strict protocols. This may include a treatment bought over the counter such as a cream or ointment, advice for self-care or supplying a prescription only medicine, such as an antibiotic or antiviral.
Secretary of State for Health and Social Care, Victoria Atkins, said:
“I’m determined to deliver faster, simpler, fairer access to care for patients, and the expansion of Pharmacy First will mean patients can get treatment for common conditions without needing to see their GP first.
“This is good news for patients and good news for the NHS. It will free up millions of GP appointments per year and mean that patients can get quick and effective treatment from their local pharmacy.
“As four in five people live within a 20-minute walk of a pharmacy, for many seeing their local pharmacist will be the easiest option – so this initiative will have real benefits for patients and help cut NHS waiting lists.”
Across England, 95% of pharmacies will be offering the expanded services, helping to delivering on our vision to support community pharmacists to evolve further into a more clinically focused role, with members of the public able to take full advantage of their skills and capabilities.
Making greater use of clinical skills in community pharmacy will offer a welcome boost to support our GPs and patients by releasing around 10 million GP appointments per year.
Pharmacy First will be integrated into the NHS website, so when people look for certain symptoms that cover Pharmacy First they will be signposted to a pharmacy.
Primary Care Minister Andrea Leadsom, said:
“When suffering from conditions like sore throat or earache, we know that patients want to be able to access the care they need quickly.
“Pharmacy First gives you choice, and the ability to be seen faster to get the care you need, providing easier and quicker access.”
The Government has a clear plan to back the pharmacy workforce. The NHS Long Term Workforce Plan commits £2.4 billion to fund additional education and training places over the next five years. This includes an ambition to increase training places for pharmacists across England by nearly 50 percent to around 5,000 by 2031/32, and to grow the number of pharmacy technicians.
NHS England has also invested £15.9 million on pharmacy professional career development. NHS England and the Centre for Pharmacy Postgraduate Education offer a range of support to upskill the current workforce with clinical examination skills.
From 2026 all newly qualified pharmacists will be independent prescribers on the day of registration. This will equip pharmacists with the skills and knowledge to provide even more clinical care and expand the clinical role of pharmacists across the NHS including in community pharmacy. I look forward to working with the sector to build further on Pharmacy First to use these new skills to benefit patients.
Community pharmacies already play a vital role in keeping their local communities healthy and well - and this role has been increasing in recent years. In 2019, the Government set out how it would work to embed and integrate community pharmacy into the NHS, delivering more clinical services and making them the first port of call for many minor illnesses. It has already made good progress, for example:
- General practice, NHS111 and Urgent and Emergency Care (UEC) can now refer patients to community pharmacies for advice and treatment for minor illnesses, and NHS111 and UEC can also refer for urgent medicines supply. Over 3.4 million referrals have been made through these routes to date.
- The Government expanded the New Medicine Service which supports over 200,000 people a month when they start new medicines and introduced the Discharge Medicine Service which supports 8,000 patients a month who have had their medicines changed following a visit to hospital, reducing medication errors and readmissions.
- Over 9,000 pharmacies have delivered over 2 million blood pressure checks since October 2021, allowing those with high blood pressure to be identified and referred for onward management. The recovery plan has made funding available for 2.5 million additional checks. It is estimated this could prevent over 1,350 cardiovascular events such as heart attacks and strokes in the first full year of service, and could lead to savings of around £13 million across primary, secondary and social care.
- It introduced a contraception service in April 2023 to enable community pharmacists to manage oral contraception on the basis of an existing prescription and in December 2023 this service was expanded so that pharmacists can now also initiate oral contraception. The recovery plan has made more funding available for this service so that up to half a million women will be able to access oral contraception through their pharmacy.
Amanda Pritchard, NHS chief executive, said:
“GPs are already treating millions more people every month than before the pandemic, but with an ageing population and growing demand, we know the NHS needs to give people more choice and make accessing care as easy as possible.
“People across England rightly value the support they receive from their high street pharmacist, and with eight in ten living within a 20-minute walk of a pharmacy and twice as many pharmacies in areas of deprivation, they are the perfect spot to offer people convenient care for common conditions.
“This is great news for patients – from today you can pop into one of more than 10,000 high street pharmacies in England to get a consultation on seven common conditions including ear-ache, a sore throat or sinusitis at a convenient time, with many pharmacies open late into the evening.
“This is all part of major transformation in the way the NHS delivers care, with the health service determined to giving people more choice in how they can access treatment.”
Now Pharmacy First will go even further, building on this success and empowering pharmacists to use their expertise to, delivering a major boost to primary care access.



